An Israeli medtech company is using artificial intelligence to help oncologists decide the best and most effective course of treatment for their cancer patients.
OncoHost’s main focus is on treatments for non-small cell lung cancer (NSCLC). According to the World Cancer Research Fund, lung cancer is the second most common cancer (after breast cancer) and responsible for 12.2 percent of new cases of the disease.
In fact, OncoHost CEO Ofer Sharon tells NoCamels, lung cancer “is the number one killer” among patients with this form of the disease.
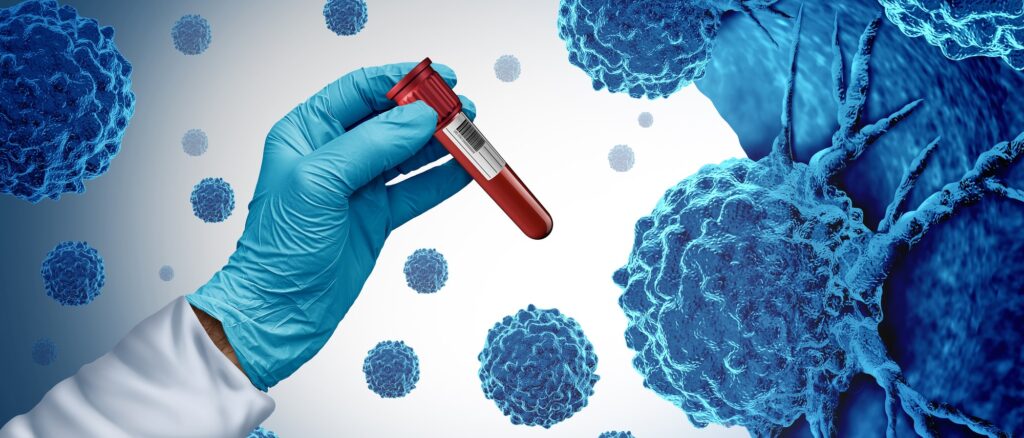
The startup’s proprietary PROphet platform uses AI to scan up to 7,000 proteins in a patient’s blood, using a single test, to see how receptive that person would be to immunotherapy to treat their tumors.
“Those proteins are telling a story about the biology of the cancer, the biology of the immune system and the biology of the resistance mechanisms,” Sharon says.
“Those same proteins are the basis of our algorithm; they also allow us to differentiate between patients who will benefit from treatment and those who won’t.”
PROphet has a two-fold purpose, Sharon explains. First, it determines whether a patient will benefit from the treatment based on the test of the proteins in the blood.
Secondly, if the patient is suitable for immunotherapy, the platform can help the doctors decide whether to pursue that as a sole treatment or to combine it with chemotherapy in order to optimize the chances of a positive outcome.
“[This is] a frequent, almost daily dilemma that oncologists are dealing with in lung cancer,” he says.
“When you start treatment, you have several options and it’s really important. There are several studies showing that the treatment you choose in the first line has a huge impact on the patient’s actual overall survival over time,” he explains.
“So it’s very important to choose right from the beginning.”
The platform tests for proteins that have been present in the blood plasma of patients who did not respond to immunotherapy but are not present for patients who did.
Sharon calls proteins “the building blocks of the biological processes in the body,” explaining that each one present in the blood plasma has a biological reason for being there.
By identifying those proteins, he explains, OncoHost can begin to understand which biological pathways are actually driving the resistance to immunotherapy, which is based on encouraging the body’s immune system to attack cancer cells.
Sharon says that while immunotherapy is the largest growing sector of cancer therapies in the last eight years, being used to treat almost every form of the disease, there have only been “moderate” clinical results.
“It is a great improvement compared to what we had 20 years ago, but we are at a point where in lung cancer only 20 to 30 percent of the patients will actually benefit from [immunotherapy] treatment,” he says.
“Immunotherapy or immunotherapy combined with chemo, it doesn’t really matter,” he explains. “Most patients are not benefiting from treatment and we really don’t understand why.”
PROphet is based on the research of Prof. Yuval Shaked, Chief Scientific Advisor at OncoHost; head of the Integrated Cancer Center at the Technion – Israel Institute of Technology in Haifa; and president of the International Cancer Microenvironmental Society, which works to advance new treatments for the disease.
Sign up for our free weekly newsletter
Subscribe
Shaked’s research for the past decade has focused on how the body’s response to treatment for cancer is critical to the patient’s ability to benefit from it. Sharon says that this is a massive change in how oncologists perceive the treatment of the disease, where previously only the interaction between the tumor and the therapy had been examined.
“When you look at cancer, there are actually three elements that take part in this interplay: the patient, the tumor and the treatment,” Sharon says. “How our own body responds to the anti-cancer treatment plays a critical role in our ability as patients to benefit from the treatment.”
Sharon says that proteins play a major role in three central hypotheses on why immunotherapy does not work in many patients:
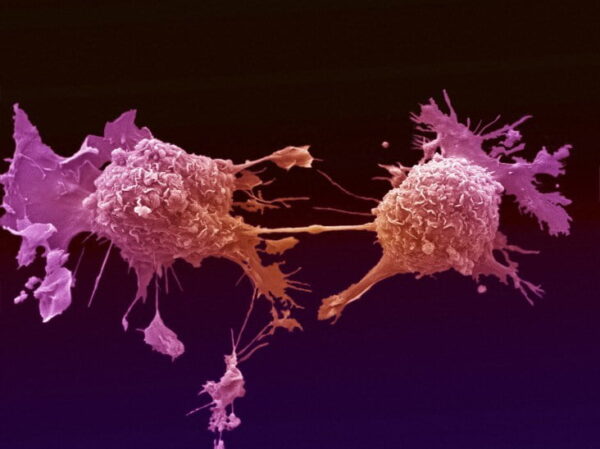
The immune system itself may be reluctant to attack the cancer cells due to the threat to healthy surrounding cells; tumors, which require a great deal of nutrients to grow, create their own blood vessels to increase their “food” supply; and the rapid proliferation of cancer cells within the body.
“We see proteins that are involved in pathways that belong to the immune system, in pathways that belong to cell proliferation and the time involved in the creation of new blood vessels, and that gives us a direction as to why the patient is not benefiting from the treatment,” he explains.
Sharon believes that the Binyamina-based startup is the only medtech company in Israel currently working on the impact of proteins on cancer treatment, simply because it is an extremely complex line of research.
“How to measure, how to understand what you see is a tool that requires a lot of integration of a lot of data points from different sources,” he says.

And while there are others working on the same premise around the world – he calls proteins “the next frontier in immunotherapy” – OncoHost is one of the most advanced in its progress.
“Right now, the tool is based on predictive algorithms,” Sharon says. The company uses mathematics, system biology and bioinformatics to tell the clinician whether the patient will benefit from the treatment or not.
“We do that with very good accuracy,” he says.
PROphet is currently undergoing clinical trials in 40 locations in Europe, Israel and the US. A version of the test has also been made accessible to clinicians in the US. The test does not require approval from the US Food and Drug Administration and those certifications that are required have been obtained.
The startup is not funded by any of the major pharmaceutical companies, which Sharon says are also involved in their own research in the field.
“This is a private company sponsored by investors – venture capital investors and other investors,” he says.
The next step, which the company has been working on for several years, is to use its understanding of the proteins found in the pathways to guide later treatment methods should the cancer progress, and even perhaps find specific treatments that block specific resistance mechanisms.
This will ultimately mean creating a personalized treatment for each patient, based on the makeup of their blood and the proteins in it.
“Clinicians don’t need a tool that will tell them to treat or not treat the patient,” Sharon says. “They need a tool that will tell them how to treat the patient.”
Related posts

Editors’ & Readers’ Choice: 10 Favorite NoCamels Articles

Forward Facing: What Does The Future Hold For Israeli High-Tech?

Impact Innovation: Israeli Startups That Could Shape Our Future



Facebook comments